23 Y/O WITH FEVER AND THROMBOCYTOPENIA
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
A 23 year old male who is a computer operator by occupation, resident of Nakrekal came to the OPD with
CHIEF COMPLAINTS :
- fever since 7 days
- pain abdomen since 7 days
HISTORY OF PRESENTING ILLNESS :
Patient was apparently asymptomatic 7 days ago,then he developed fever (99F) which is abrupt onset, continuous and not associated with chills,headache with no aggravating factors and was relieved temporarily on taking paracetamol and he developed abdominal pain which was sudden onset, gradually progressive, not localized, but pain is more around umbilical area and right hypochondrium area
h/o nausea and vomitings-2 episodes on day2 of fever
h/o rash over inner thighs, non-pruritic in nature, not associated with any pain, no aggravating and relieving factors
h/o redness of the eyes yesterday
PAST HISTORY:
no history of diabetes, hypertension, asthma, epilepsy, tb, thyroid disorders
h/o polio since birth
PERSONAL HISTORY:
He takes mixed diet, decreased appetite, sleep was normal, bowel movements were irregular(4times weekly),constipation since 4 days and bladder movements were regular, no addictions.
TREATMENT HISTORY: n/a
ALLERGIC HISTORY: n/a
GENERAL EXAMINATION:

INVESTIGATIONS:
PROVISIONAL DIAGNOSIS: DENGUE HEMORRHAGIC FEVER
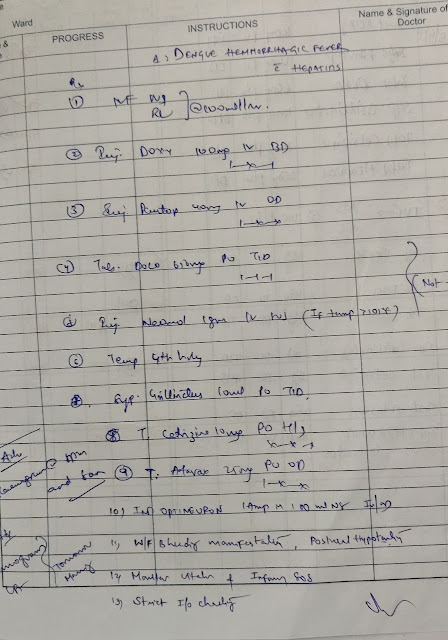
TREATMENT:







Comments
Post a Comment